Visits to the doctor are often spaced out by weeks or months and usually limited to 15 minutes or less. Although experienced healthcare providers have developed a keen ability to detect how a patient is doing in this brief snapshot, a particularly good or bad day for the patient can bias the assessment. Moreover, the status of patients with serious illness and those undergoing aggressive treatments can shift rapidly. Important changes in individual functioning may not be brought to the attention of the healthcare team in a timely fashion, and often patients are not aware of which symptoms reveal important disease-related changes. Yet, a patient’s level of functioning, or performance status, is one of oncology’s vital signs, as it is a key factor in decisions about the patient’s treatment. The explosion of low-cost, real-time data collection technologies is being embraced as creating a possible means to bridge the information gap between office visits and to allow for more systematic and comprehensive patient monitoring of performance status.
The Center for Self-Report Science (CSS) within the Center for Economic and Social Research (CESR) is part of a multidisciplinary team spanning the USC Dornsife College of Letters, Arts and Sciences, the USC Michelson Center for Convergent Bioscience, the USC Norris Comprehensive Cancer Center, and the USC Viterbi School of Engineering. Psychologists, biophysicists, oncologists, and engineers have come together for the Analytical Technologies to Objectively Measure Human Performance (ATOM-HP) project, which is testing the feasibility and utility of a multi-sensor framework for improving cancer patient care through continuous monitoring.
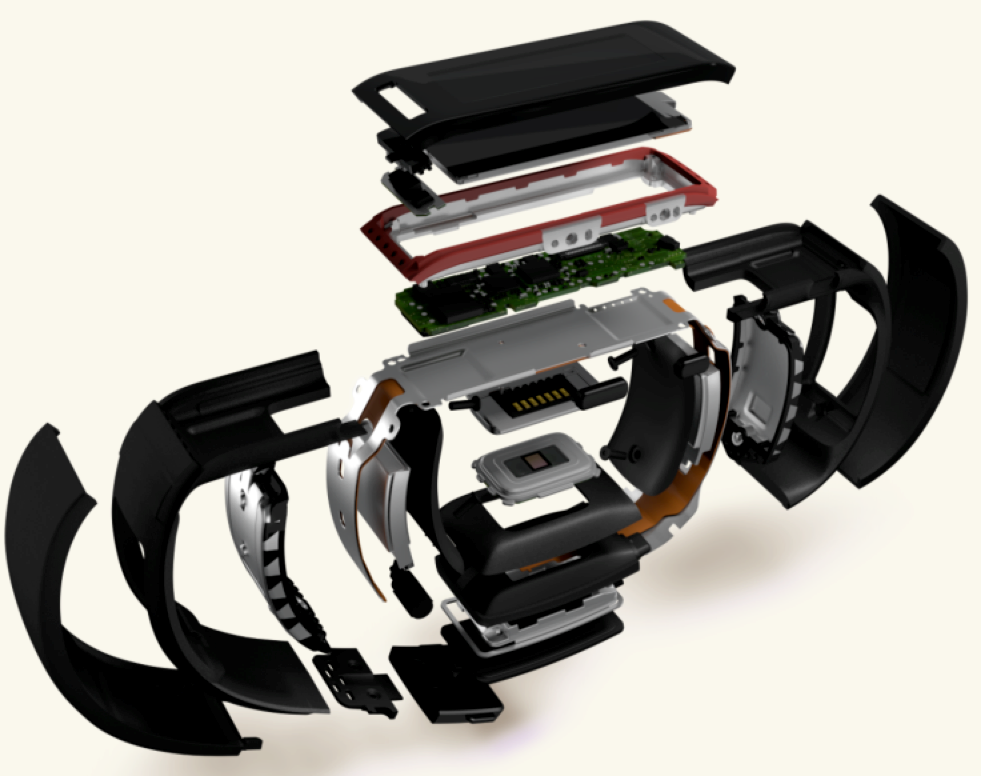
ATOM-HP is currently involved in a trial of objective, longitudinal monitoring of cancer patients undergoing chemotherapy treatment. As part of the trial, different devices are used to monitor and measure various indicators of a patient’s functioning. A Microsoft Kinect, a depth imaging device originally manufactured for use with home video game consoles, assesses the patient’s posture and gait, and the speed with which the patient sits, stands, and moves during doctor’s office visits. Between visits, patients report on key symptoms on a daily basis with validated Patient-Reported Outcome Measurement Information System (PROMIS®) scales. They also wear a Microsoft Band to track their heart rate and activity levels.
The Microsoft Kinect, PROMIS® scales, and the Microsoft Band came into being well before ATOM-HP. “We didn’t invent wearable accelerometers, we didn’t invent movement trackers, we didn’t invent patient-reported outcomes,” says Jorge Nieva, M.D., one of the lead researchers. “So, when one looks at the project, one might say we’re not really inventing anything. Yet, what we did is we took these tools that were already available and applied them to a real problem, in a way that patients and caregivers could all understand.” To that end, machine learning algorithms are being utilized to integrate the information collected from these separate devices with the goal of providing highly accurate assessments of the patient’s performance status. These data will then be used in prediction models of patient treatment response.
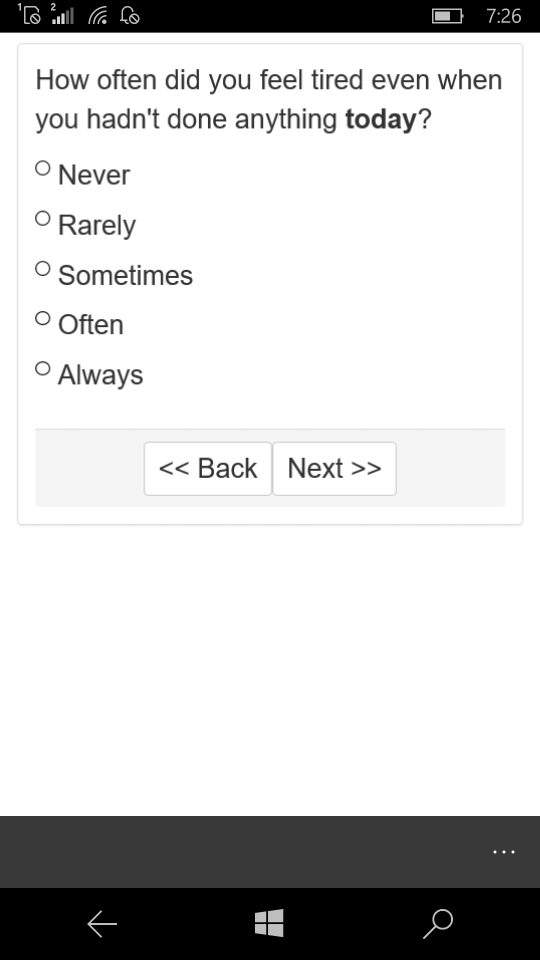
CSS spearheads the collection of patient-reported outcomes for ATOM-HP. Joan Broderick, Ph.D., Associate Director of CSS and a principal investigator within the National Institutes of Health PROMIS Roadmap Initiative, compiled the scales for the project. Social Isolation is assessed at baseline, Fatigue, Sleep Disturbance, and Physical Function are assessed each week, and Fatigue and Appetite are assessed on a daily basis. Questions are delivered to the patient through a smartphone app designed specifically for this purpose. In addition to Fatigue and Appetite items, the app asks patients to enter their weight and take a selfie; the selfies are then analyzed by computer scientists involved in the measurement of facial expressions and recognition of human emotions.
 On October 3, ATOM-HP was showcased at South by South Lawn: A White House Festival of Ideas, Art, and Action (SXSL). An interactive booth allowed attendees to immerse themselves in the patient experience by engaging with the technologies and transmitting their data to the on-site oncologist in real time. In the weeks since, the project has been championed as a strategy to catalyze new scientific breakthroughs by Vice President Joe Biden’s Cancer Moonshot initiative. ATOM-HP hopes to make use of this national exposure to appeal to policymakers to change the way healthcare laws are written, allowing for a transition from episodic to ‘continuum care’. Although still in clinical trials, ATOM-HP is thinking ahead.
On October 3, ATOM-HP was showcased at South by South Lawn: A White House Festival of Ideas, Art, and Action (SXSL). An interactive booth allowed attendees to immerse themselves in the patient experience by engaging with the technologies and transmitting their data to the on-site oncologist in real time. In the weeks since, the project has been championed as a strategy to catalyze new scientific breakthroughs by Vice President Joe Biden’s Cancer Moonshot initiative. ATOM-HP hopes to make use of this national exposure to appeal to policymakers to change the way healthcare laws are written, allowing for a transition from episodic to ‘continuum care’. Although still in clinical trials, ATOM-HP is thinking ahead.
Leveraging modern technologies to continuously monitor patients has broad implications for both research and practice. Access to real-time data from multiple sources, instantly integrated and analyzed, could be relevant to oncology healthcare providers who see the lack of timely information as an obstacle. In practice, this integrated, analyzed data would give healthcare providers an objective view of their patient’s status across time, making the impact of treatment apparent and speeding up treatment course corrections.
This detailed, objective assessment of patient performance status parallels recent advances in individual genotyping of the patient’s tumor to create a treatment plan that will work best for that specific patient. Historically, medical treatments were designed for the ‘average’ patient, based on the results of clinical trials of groups of patients. This one-size-fits-all approach is fading as the unique characteristics of each patient’s tumor and performance status are factored into treatment approaches. President Barack Obama’s Precision Medicine Initiative ($215 million in fiscal year 2016) is designed to take variability in genes, environment, and lifestyle into account by tailoring disease prevention and treatment approaches to the individual patient.
Importantly, ATOM-HP also has the potential to be deployed across the socioeconomic spectrum. “Done smartly, it can be packaged to be self-contained; programmed appropriately, it can operate across languages and cultural backgrounds,” writes Peter Kuhn, Ph.D., one of the project lead researchers.
ATOM-HP is currently enrolling patients at sites in California (Los Angeles, Newport Beach) and Texas (Houston).
For more information, please see additional articles about ATOM-HP in The Hill and USC’s Press Room.
You must be logged in to post a comment.